The COVID-19 pandemic has brought about numerous health challenges worldwide. While the virus primarily targets the respiratory system, emerging evidence suggests it can affect other vital organs, including the heart, in the long term. Medical professionals have observed a concerning surge in the incidence of ischaemic heart disease (IHD) following COVID-19 infections. This article explores the relationship between COVID-19 and IHD and delves into potential mechanisms contributing to this worrisome trend.
“Impact of COVID-19 on Patients with ST-Elevation Myocardial Infarction: Insights from a British Cardiac Specialist Centre” (Kunadian et al., 2020): The study focused on patients with ST-elevation myocardial infarction (STEMI) and revealed an increased delay in seeking medical care and a higher mortality rate during the COVID-19 pandemic compared to the pre-pandemic period.
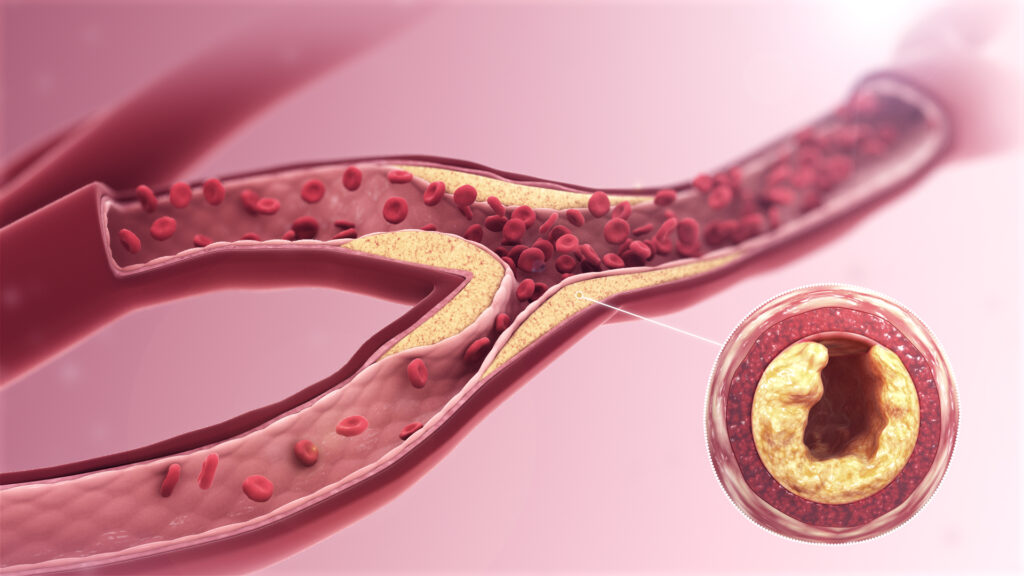
Understanding Ischaemic Heart Disease:
Ischaemic heart disease, or coronary artery disease, occurs when the coronary arteries that supply blood to the heart muscle become narrowed or blocked. It is the leading cause of death globally and is often associated with risk factors such as hypertension, high cholesterol, smoking, diabetes, and obesity. The condition manifests as chest pain (angina), heart attacks, or heart failure.
COVID-19 and Ischaemic Heart Disease:
Studies have revealed a significant increase in the incidence of IHD in individuals who have contracted COVID-19. A retrospective analysis of patient data found a higher prevalence of acute coronary syndromes, myocardial infarctions, and heart failure in COVID-19 patients compared to the general population. The link between COVID-19 and IHD is multifactorial and can be attributed to several factors.
1. Inflammation and Endothelial Dysfunction:
COVID-19 triggers a systemic inflammatory response in the body. This heightened inflammatory state can lead to endothelial dysfunction, which impairs blood vessels’ functioning and promotes blood clots’ formation. These blood clots can occlude the coronary arteries, resulting in myocardial infarction.
2. Direct Viral Infection:
The SARS-CoV-2 virus can directly invade the heart muscle cells, causing myocarditis (inflammation of the heart) or myocardial injury. This damage weakens the heart and increases the risk of IHD.
3. Exacerbation of Pre-existing Conditions:
Individuals with pre-existing cardiovascular conditions, such as hypertension or atherosclerosis, are at a higher risk of severe COVID-19 infection. The virus can exacerbate these underlying conditions, leading to increased incidences of IHD.
4. Psychological Stress:
The psychological stress associated with the pandemic, including anxiety, fear, and social isolation, can contribute to developing or worsening IHD. These factors can increase blood pressure, trigger arrhythmias, and disrupt cardiovascular health.
Long-Term Implications:
The long-term consequences of COVID-19-related IHD are a cause for concern. Survivors of severe COVID-19 infections may experience lingering cardiovascular damage, resulting in chronic heart conditions, reduced quality of life, and increased mortality rates. Additionally, the burden on healthcare systems due to the rising number of IHD cases places additional strain on resources already stretched by the pandemic.
Mitigating the Risk:
To mitigate the risk of developing IHD following COVID-19, several measures can be taken:
1. Vaccination: Widespread vaccination campaigns are crucial in reducing the overall impact of COVID-19 and potential cardiac complications.

2. Post-COVID Follow-up: Individuals who have recovered from COVID-19, particularly those who experienced severe illness, should undergo regular cardiac check-ups to monitor for any signs of IHD.
3. Healthy Lifestyle: Adopting a healthy lifestyle, including regular exercise, a balanced diet, smoking cessation, and stress management, can help prevent and manage IHD.
4. Mental Health Support: Providing psychological support and resources to individuals experiencing pandemic-related stress and anxiety can alleviate the burden on the cardiovascular system.
Conclusion:
The correlation between COVID-19 and the increased incidence of ischaemic heart disease is alarming, and the multifaceted relationship between the virus and IHD requires further research and understanding. As we navigate the post-pandemic era, it is crucial to prioritise cardiovascular health and implement preventive measures to mitigate the long-term impact of COVID-19 on heart health.



Be the first to comment